Spontaneous coronary artery dissection (SCAD) is an infrequent and often missed diagnosis especially in women presenting with acute coronary syndrome (ACS).
SCAD is defined as a non-traumatic and non-iatrogenic separation of the coronary arterial walls, creating a false lumen (1). This separation can occur between the intima and media or between the media and adventitia, with intramural hematoma (IMH) formation within the arterial wall that compresses the arterial lumen, decreasing antegrade blood flow and subsequent myocardial ischemia or infarction (1,2).
There are two proposed mechanisms for the formation of IMH with SCAD. The first involves an intimal tear resulting in blood from the endoluminal space entering the intimal space, creating a false lumen filled with blood.
The second mechanism of IMH formation is thought to be due to rupture of the vasa vasorum, which are small arterioles within the walls of arteries supplying blood to the walls. When such rupture occurs, blood can pool within the intramural space, creating a false lumen filled with hematoma. Figure 1 shows the distinctive features between the two mechanisms (1).
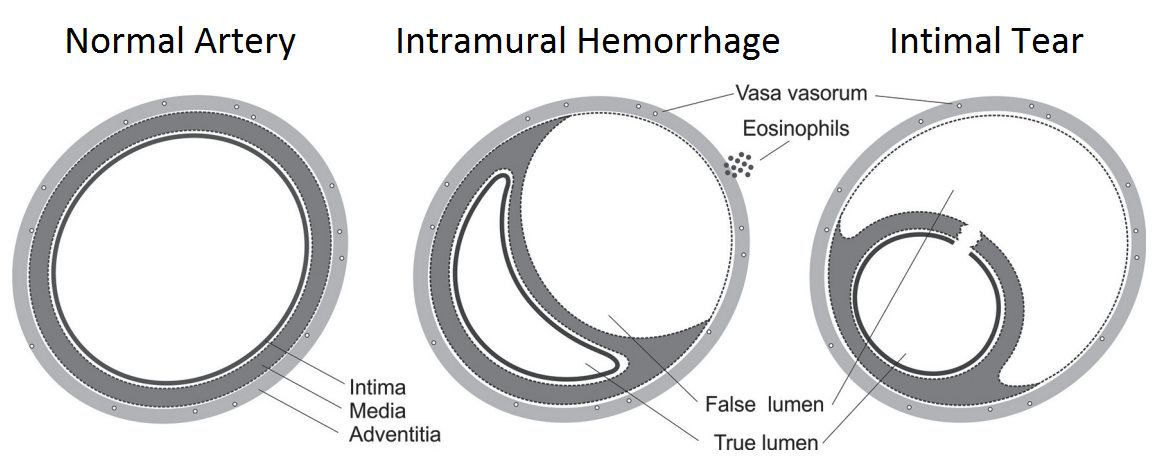
Figure 1: Schematic diagram of the mechanisms of spontaneous coronary artery dissection. Reproduced with permission from (1).
Clinically, the mechanism of the tear is probably unimportant, and coronary angiography is notoriously suboptimal to visualize intimal tears.
The usual pathogenesis of ACS involves atherosclerotic plaque rupture that is distinct from non-atherosclerotic forms of SCAD. Dissections due to atherosclerosis tend to be less extensive, as medial atrophy and scarring from atherosclerosis limits propagation of the dissection (1).
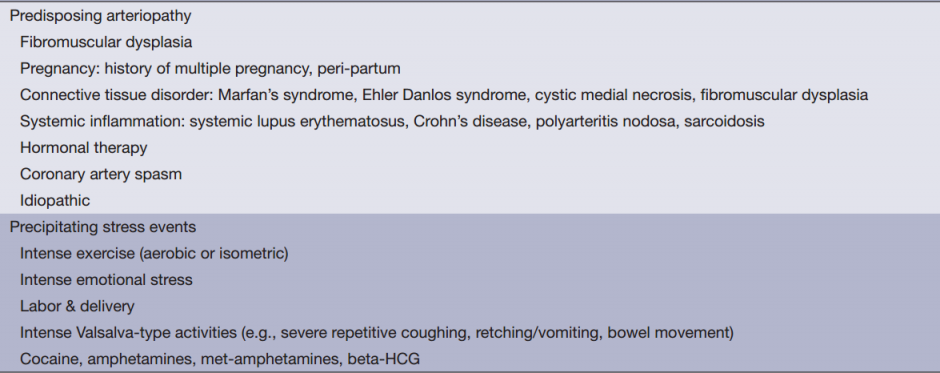
Non-atherosclerotic SCAD is typically a culmination of disease pathways that predispose arterial beds to injury. These include fibromuscular dysplasia (FMD), multiple pregnancy, systemic inflammation (systemic lupus erythematosus, Crohn’s disease, polyarteritis nodosa and sarcoidosis), connective tissue disorder (Marfan’s syndrome, Ehler Danlos, cystic medial necrosis), hormonal therapy, and coronary artery spasm (Table 1).
Table 1: Etiology of non-atherosclerotic SCAD
References:
1. Saw J. Spontaneous coronary artery dissection. Can J Cardiol 2013;29:1027-33.
2. Vrints CJ. Spontaneous coronary artery dissection. Heart 2010;96:801-8.