SCAD is a spontaneous, non-traumatic, and noniatrogenic separation of the coronary artery wall by intramural hemorrhage, which can occur with or without an inciting intimal tear. The creation of a false lumen with intramural hematoma (IMH) can propagate antegrade and retrograde, compressing arterial lumen to varying degrees, and causing ischemia or infarction according to the degree of arterial occlusion. There are two proposed mechanisms for SCAD. The first is an intimal tear that leads to hemorrhage into the media, causing medial dissection and creation of a false lumen. This may appear angiographically as the pathognomonic multiple radiolucent lumen, contrast dye stains in the arterial wall, or slow clearing or hang-up of contrast dye in the lumen. The second mechanism is less well known, and is proposed to be initiated by the rupture of vaso vasorum causing spontaneous bleed into arterial wall producing IMH [1]. This may appear only as luminal compression, and this angiographic appearance is more commonly seen than the classic arterial wall stains [2]. Most angiographers are not familiar with this nonclassic angiographic appearance of SCAD, contributing to why SCAD is often missed on angiograms. Other reasons include mild stenosis, smooth-walled stenosis, and involvement of distal and small arteries.
It is difficult to ascertain the true prevalence of SCAD as it is often under-diagnosed and has varying presentations from mild chest pains to sudden cardiac death.
Challenges of diagnosis: (1) Low index of clinical suspicion, (2) Coronary angiogram is an imperfect test (2-dimensional depiction of 3-dimensional arteries, luminogram, cannot image arterial walls), (3) Angiographers sole reliance of pathognomonic SCAD angiographic findings, (4) Unfamiliarity with angiographic variants of SCAD, (5) Insufficient use of IVUS or OCT.
Angiographic Variants of SCAD: Appearance
There are three distinct angiographic appearances and patterns of SCAD that can be characterized:
1. Angiographic Variant Type 1: Evident Arterial Wall Stain.
This is the pathognomonic angiographic appearance of SCAD with contrast dye staining of arterial wall with multiple radiolucent lumen.
Type 1- Patient A: Right Posterior Descending Artery (RPDA) Spontaneous Coronary Artery Dissection (SCAD)
Type 1 – Patient A: RPDA SCAD Healed after 6 Weeks
Type 1 – Patient B: Left second obtuse marginal (OM2) coronary artery SCAD
Type 1 – Patient C: Left anterior descending artery (LAD) SCAD
Type 1 – Patient C: Right renal fibromuscular dysplasia (FMD)
Type 1 – Patient D: Right posterolateral branch of the right coronary artery (RPL) SCAD
Type 1 – Patient D: Right renal (FMD)
2. Angiographic Variant Type 2: Diffuse Stenosis of Varying Severity
This angiographic appearance is not well appreciated and is often missed or misdiagnosed. SCAD commonly involves the mid to distal segments of coronary arteries, and can be so extensive that it reaches the distal tip. There is an appreciable (often subtle) abrupt change in arterial caliber, with demarcation from normal diameter to diffuse narrowing. This diffuse (typically >20 mm) and usually smooth narrowing can vary in severity from an inconspicuous mild stenosis to complete occlusion.
Type 2 – Patient E: OM2 coronary artery SCAD
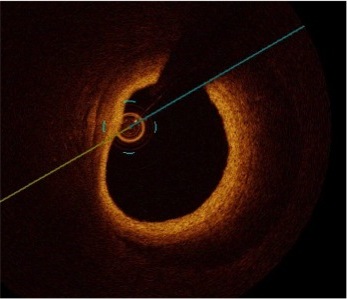
Type 2 – Patient E: Optical Coherence Tomography (OCT) of OM2 coronary artery SCAD
Type 2 – Patient E: FMD of both renal arteries
Type 2 – Patient E: FMD of left iliac artery
Type 2 – Patient F: RPL SCAD
Type 2 – Patient F: RPL SCAD healed 7 weeks later
Type 2 – Patient G: RPL SCAD
Type 2 – Patient G: RPL SCAD healed 7 months later
Type 2 – Patient H: First obtuse marginal (OM1) coronary artery SCAD
Type 2 – Patient H: OM1 coronary artery SCAD healed 10 months later
Type 2 – Patient H: Left renal FMD
Type 2 – Patient I: LAD SCAD
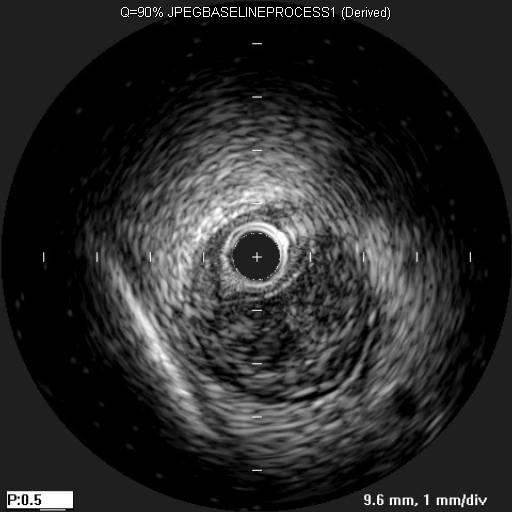
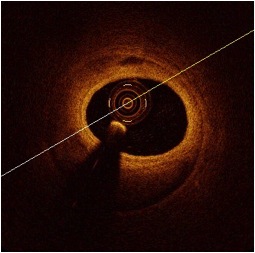
Type 2 – Patient I: IVUS image of LAD SCAD
Type 2 – Patient J: Ramus intermedius branch SCAD
Type 2 – Patient J: Ramus intermedius branch SCAD healed 17 months later
Type 2 – Patient K: LAD SCAD
Type 2 – Patient K: LAD SCAD healed 3 months later
Type 2 – Patient L: RPDA SCAD
Type 2 – Patient L: RPDA SCAD healed 6 years later
Type 2 – Patient M: Right coronary artery (RCA) SCAD
Type 2 – Patient M: RCA SCAD healed 7 weeks later
Type 2 – Patient M: Left renal FMD
Type 2 – Patient M: Right renal FMD
Type 2 – Patient N: LAD SCAD
Type 2 – Patient N: LAD SCAD healed 3 months later
3. Angiographic Variant Type 3: Mimic Atherosclerosis
This appearance is the most challenging to differentiate from atherosclerosis and most likely to be misdiagnosed. Angiographic features that favor SCAD are: (i) lack of atherosclerotic changes in other coronary arteries; (ii) long lesions (11-20 mm); (iii) hazy stenosis; and (iv) linear stenosis. Angiographer needs to have a high index of suspicion for SCAD and employ intracoronary imaging for such cases.
Type 3 – Patient O: Mid LAD SCAD
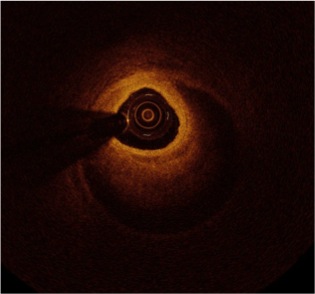
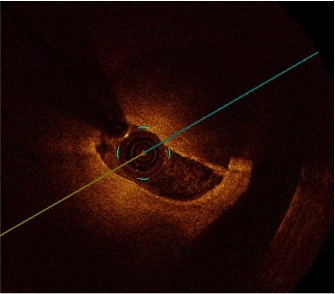
Type 3 – Patient O: OCT of LAD SCAD
Type 3 – Patient P: LAD SCAD
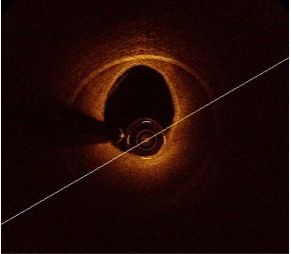
Type 3 – Patient P: OCT of LAD SCAD
Type 3 – Patient Q: LAD SCAD
Type 3 – Patient Q: OCT of LAD SCAD
Type 3 – Patient R: OM1 SCAD
Type 3 – Patient R: OCT of OM1 SCAD